
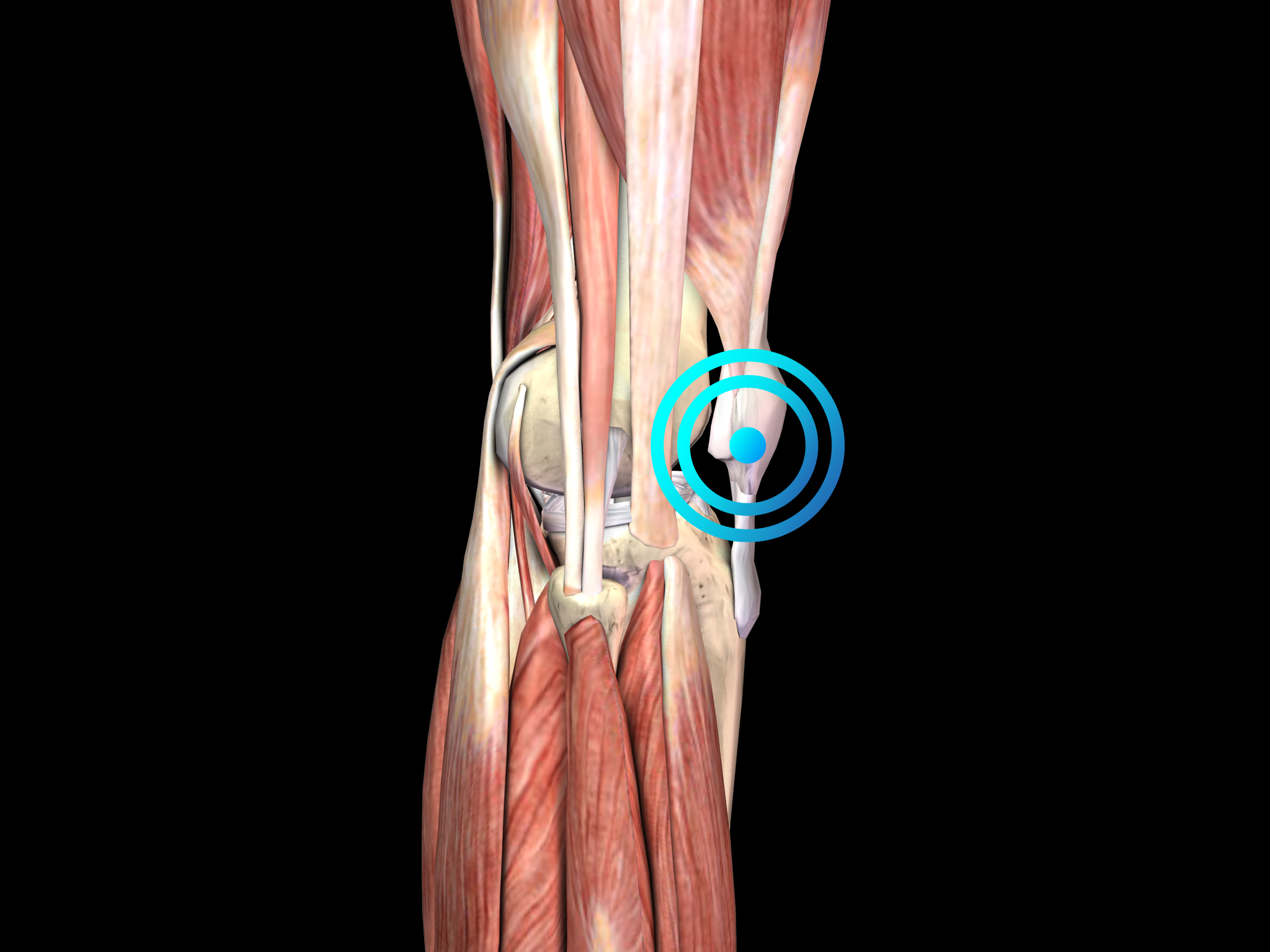
Patella tip syndrome
Pathology
The main clinical symptom is pain at the inferior pole of the patella. Diagnosis is based on the clinical features of the disease. Diagnostic imaging should be considered to rule out other causes of knee pain or to establish the diagnosis of patella tip syndrome when in doubt.
Similar to other tendinopathies, the etiology of patella tip syndrome is not completely understood, but repetitive overload is thought to be an important factor. Histologic examination of biopsy specimens from patients undergoing patellar tendon surgery for chronic symptoms has shown that chronic PT is associated with degenerative changes in the tendon. Accordingly, the disease is better characterized as “tendinopathy” than “tendinitis”, resembling the situation in other overuse tendon problems such as Achilles tendinopathy.
Athletes have a very high prevalence of jumper`s knee, i.e., up to 40% among elite basketball and volleyball players.
The condition can be debilitating and may prevent athletes from returning to sport for long periods between 6 months and more than 2 years.
The treatment of patella tip syndrome should start with conservative treatment modalities including rest, physiotherapy, eccentric strengthening, bracing and non-steroidal anti-inflammatory drugs.
Patients not responding to conservative treatment for six months should then undergo radial shock wave therapy for the treatment of patella tip syndrome.
Surgery should be considered for recalcitrant cases of patella tip syndrome. Numerous arthroscopic and open procedures have been described, but a consensus agreement about the best option is not available.
Side effects of Radial Shock Wave Therapy (RSWT) using the Swiss DolorClast®.
When performed properly, RSWT with the Swiss DolorClast® has only minimal risks. Typical device-related non-serious adverse events are:
- Pain and discomfort during and after treatment (anaesthesia is not necessary)
- Reddening of the skin
- Petechia
- Swelling and numbness of the skin over the treatment area
These device-related non-serious adverse events usually disappear within 36h after the treatment.
Treatment Procedure
Locate the area of pain through palpation and biofeedback.
Mark the area of pain.
Apply coupling gel to transmit shock waves to the tissue.
Deliver Radial or Focused Shock Waves to the area of pain while keeping the applicator firmly in place on the skin.
Clinical proof
Practitioner?
Get information on the diagnosis, the functioning of shock wave therapy, clinical proof, contraindications, etc.


